Medical Waste Recycling: Sterilization and Safety Protocols
Discover the innovative methods transforming medical waste recycling, focusing on sterilization tech, healthcare metals recovery, and biohazard management to ensure sustainability and safety
WASTE-TO-RESOURCE & CIRCULAR ECONOMY SOLUTIONS
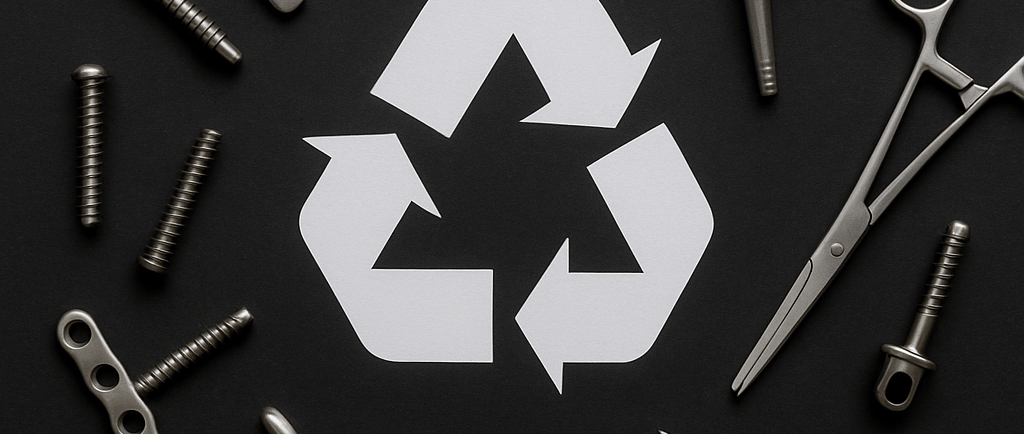

Introduction: Turning Clinical Waste into Sustainable Value
The healthcare industry stands at the crossroads of cutting-edge innovation and significant environmental responsibility. Medical waste management, traditionally regarded as a backend operation, is experiencing a paradigm shift. The volume of waste generated by global healthcare facilities is staggering — the World Health Organization (WHO) estimates that high-income countries produce up to 0.5 kg of hazardous waste per hospital bed per day. Among these materials lies a hidden asset: valuable metals embedded within surgical tools, orthopedic fixations, dental components, and diagnostic equipment.
These structural metals — including stainless steel, titanium, cobalt-chromium alloys, and aluminum — are resource-intensive to produce from virgin ore. However, by unlocking this "urban mine" through recycling, hospitals can slash carbon emissions, reduce landfill burden, and actively contribute to the circular economy.
Yet, medical metal recycling is not plug-and-play. Due to contamination with infectious agents, body fluids, and complex material structures, it demands specialized sterilization, strict adherence to safety protocols, and regulatory oversight. Moreover, the rise of precision-engineered healthcare devices has made metal separation more technical and nuanced than ever before.
This comprehensive guide dives deep into how sterilization technology, stringent safety standards, and a renewed sustainability mindset are converging to reshape medical waste recycling — transforming biomedical liabilities into ecological opportunities.
1. Understanding the Importance of Healthcare Metal Recycling
The Unseen Value of Healthcare Metals
In the world of clinical procedures, metals are indispensable. From titanium hip implants to stainless steel scalpels, their usage is rooted in biocompatibility, corrosion resistance, and durability. These materials often remain viable long after a device has been discarded due to upgrades, expiry, or single-use application.
Consider the following commonly used metals in healthcare:
- Stainless steel: Scalpels, surgical scissors, trays.
- Titanium: Orthopedic and dental implants, surgical fasteners.
- Aluminum: Frames of wheelchairs, surgical lighting fixtures.
- Cobalt-chromium alloys: Joint replacements, stents.
- Nickel-chromium: Dental restorative tools.
These metals are not only recyclable but also hold significant residual value. Scrapping even a modest volume of titanium and stainless steel can recoup substantial costs. According to industry estimates, stainless steel scrap commands anywhere between $0.30 to $1.00 per pound, while titanium can fetch upwards of $2 to $4 per pound depending on purity and market conditions.
Environmental and Economic Significance
Recycling these metals contributes positively to sustainability on multiple fronts:
- 🌱 Energy Efficiency: Reprocessing aluminum saves up to 95% of the energy required to extract it from ore. Similarly, recycling titanium consumes over 50% less energy than refining it from raw minerals.
- 💰 Cost Mitigation: Healthcare providers spend millions annually on waste disposal. By recouping value through metal recovery, facilities can offset expenses—and, in some cases, establish new revenue streams.
- ♻️ Circular Economy Goals: As 2030 sustainability benchmarks loom closer, public and private healthcare institutions are prioritizing circular supply chains. By integrating material reuse and recycling, they align with globally recognized goals like the United Nations Sustainable Development Goal 12 (Responsible Consumption and Production).
Case in Point: Cleveland Clinic & Material Recovery
Cleveland Clinic, a top-tier U.S. hospital network, implemented a comprehensive medical device recovery program. Over five years, the program recovered more than 460,000 pounds of metal waste—including stainless steel and titanium—from surgical centers, diverting it from landfills and reducing overall operational waste.
The initiative exemplifies how healthcare entities can go beyond compliance and champion environmental stewardship through strategic recycling.
2. Challenges in Recycling Metal from Medical Waste
While the rewards are undeniable, the journey toward effective metal recycling in the medical sector is not without significant obstacles.
a. Biohazard Risks
Used medical equipment may retain contamination from pathogens like Staphylococcus aureus, Hepatitis B virus, or HIV. Even residues from bodily fluids can harbor microbial life capable of transmission. This makes improper handling or uncontrolled disposal not just a regulatory offense—but a potential public health hazard.
In fact, a 2019 report from the Centers for Disease Control and Prevention (CDC) warned that lapses in sterilization and waste handling significantly increase the risk of nosocomial (hospital-acquired) infections. This underscores the need for airtight infection control practices before any recycling can occur.
b. Material Complexity
Modern medical devices are marvels of medical engineering. Yet, their complexity is a double-edged sword when it comes to recycling. Instruments often combine multiple substrates — such as plastics for ergonomic support, synthetic rubbers for insulation, or specialized coatings for chemical resistance — which complicate metal recovery.
For instance, an electrocautery pencil might house:
- Stainless steel blade elements
- Plastic casing
- Copper wiring
- Silicone rubber insulation
Dismantling such devices manually is impractical at scale, while automated separation requires tailored mechatronics and material recognition software. Consequently, the economic and technological feasibility of recycling must be assessed device by device.
c. Regulatory Complexity
In the U.S., medical waste recycling falls under the jurisdiction of various federal and state agencies:
- OSHA governs workplace exposure to biohazards.
- EPA regulates handling and incineration via the Resource Conservation and Recovery Act (RCRA).
- FDA oversees reprocessing and reuse of medical devices.
Globally, variations exist. In Europe, the EU Waste Framework Directive and Medical Devices Regulation (MDR) dictate standards, while countries like India and Japan have their region-specific biomedical waste laws.
Non-compliance carries significant risks — not only fines or permit revocations but also reputational damage and risk of legal liability in case of infection outbreaks linked to poorly recycled goods.
d. Sterilization: The Gatekeeper of Recycling
Sterility protocols are the cornerstone of safe medical metal recycling. Contaminated materials must be proven pathogen-free through sterilization before any physical processing. This isn’t merely precautionary—it’s a legal and ethical mandate.
Additionally, sterilization method selection must consider material impact. Some high-temperature methods can compromise the integrity or recyclability of thermally sensitive alloys. Hence, facilities must balance effectiveness, throughput, and material compatibility in choosing the correct decontamination technology.
Let’s make sustainability in healthcare more than just a trend—it’s a necessary transformation.
Sterilization Breakthroughs, Safety Engineering, and Advanced Metal Recovery
1. Next-Generation Sterilization Technologies
Medical metal recycling hinges on effective decontamination that balances pathogen elimination with material preservation. Innovations are transforming this field:
High-Speed Steam Autoclaving 2.0:
Modern autoclaves now integrate pre-vacuum pulsed cycles and superheated steam (134–137°C) to penetrate complex instrument geometries. Advanced models feature real-time bio-indicator validation (e.g., Geobacillus stearothermophilus spores) to ensure 6-log pathogen reduction without damaging metal integrity 110.Low-Temperature Alternatives:
Microwave-Assisted Thermal Systems: Uses 2.45 GHz electromagnetic waves to generate internal heat, neutralizing pathogens in minutes. Ideal for heat-sensitive alloys like titanium-copper composites 2.
Vaporized Hydrogen Peroxide (VHP): Deploys micro-condensation technology to sterilize metals at 40–50°C, leaving no toxic residues. FDA-approved for implantable device reprocessing 12.
Ethylene Oxide (EtO) Innovations: New catalytic converters in EtO systems reduce emissions by >99.9%, addressing EPA concerns while maintaining compatibility with polymer-coated instruments 12.
Radiation Sterilization Advances:
Gamma irradiation (Cobalt-60) and E-beam systems now achieve sterility at 25–40 kGy with reduced exposure times. Stabilizer-enhanced alloys prevent oxidative degradation during treatment 812.
Sterilization method compatibility varies significantly across techniques: Steam autoclaving operates at 121–134°C and 15–30 psi, demonstrating excellent compatibility with stainless steel and titanium alloys, though only fair results with aluminum, while achieving over 6-log pathogen reduction. Vaporized Hydrogen Peroxide (VHP) functions at lower temperatures (40–50°C) and pressure, maintaining compatibility with all metals and delivering 4–6-log pathogen reduction. Gamma irradiation works at ambient temperatures, requiring stabilizers for optimal metal compatibility, but achieves greater than 6-log reduction efficacy. Ethylene Oxide (EtO) operates between 30–60°C and is universally compatible with all metal types while providing consistent 6-log pathogen reduction across materials. Each method presents distinct temperature profiles, material limitations, and microbial elimination capabilities that inform their application in medical metal recycling.
2. Safety Protocols: Protecting People and Planet
Infection control extends beyond sterilization to encompass end-to-end safety engineering:
Hierarchy of Hazard Controls:
Elimination: Automated robotic sorters (e.g., AI-guided arms) remove sharps from metal waste streams, eliminating manual handling 3.
Engineering Controls: Negative-pressure decontamination rooms with HEPA-filtered airflow (≥12 ACH) contain aerosols during shredding 610.
Administrative Measures: Blended-learning programs for staff, including VR simulations for spill response and waste segregation protocols 37.
Post-Sterilization Monitoring:
Biological Indicators (BIs): Geobacillus spore tests verify sterilization efficacy every load 10.
Chemical Indicators: Color-changing integrators on container surfaces confirm steam/radiation penetration 12.
Residual Testing: GC-MS analysis ensures EtO residues are <1 ppm before metal processing 12.
3. Metal Recovery: Engineering the Circular Loop
Recycling facilities now deploy multi-stage recovery systems to extract maximum value:
Separation Engineering:
Primary Shredding: Contamination-safe crushers with liquid nitrogen cooling prevent heat-induced metal oxidation 11.
Sensor-Based Sorting: Hyperspectral cameras and XRF analyzers identify and separate SS304 from Ti-6Al-4V fragments at 5 tons/hour 311.
Electrodynamic Fragmentation: Pulsed high-voltage discharges liberate embedded metals from plastic/ceramic composites without material loss 11.
Closed-Loop Metallurgy:
Hydrometallurgical Leaching: Selective solvents (e.g., Deep Eutectic Solvents) dissolve base metals, leaving high-value cobalt/chromium for electrolytic recovery (95% purity) 11.
Plasma Arc Smelting: 10,000°C torches vaporize impurities from surgical steel, enabling direct reuse in medical device forging 11.
Circular Product Integration:
Recycled metals re-enter healthcare supply chains as:Surgical instrument blanks (e.g., reprocessed SS316L for forceps)
Orthopedic implant substrates (Ti-64 powder for 3D-printed hips)
Hospital infrastructure (Al frames for hospital beds)
Stainless steel undergoes a recovery process combining magnetic separation, eddy current sorting, and smelting, achieving 99.2% purity for reuse in surgical trays and bone screws. Titanium alloys are processed through plasma arc smelting followed by electrorefining, reaching exceptional 99.95% purity suitable for dental implants and pacemaker casings. Aluminum is recovered through cryomilling and electrolysis, attaining 98.7% purity for applications like wheelchair frames and surgical lighting fixtures. Cobalt-chromium undergoes solvent extraction paired with electrowinning, achieving 99.8% purity for high-value reuse in joint replacements and stents. Each metal's specialized recovery pathway ensures maximum purity while enabling circular reintegration into critical healthcare applications.
The Sustainable Sterilization Ecosystem
Modern healthcare recycling merges sterilization rigor, safety-by-design, and recovery innovation to transform waste into value. Facilities like NHS Tayside have slashed CO₂ by 1,746 kg/year through closed-loop metal recycling 7, while EPA-compliant EtO systems reduce emissions to <0.1 ppm 12. Future progress hinges on:
Blockchain material tracing from waste bin to smelter
Enzymatic bio-recycling for polymer-metal hybrids
ISO 14048-compliant LCA tools to quantify carbon savings
This technical evolution positions medical facilities not just as waste generators, but as resource stewards driving the circular healthcare economy.
"Recycling one tonne of anaesthetic metal saves 1,480 kg of CO₂—equivalent to 3,500 miles driven by an average car."
— Ninewells Hospital Metal Recycling Trial
